A 18year old male patient came with the chief complaints of fever since 4 days
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitt
A 18 year old boy,resident of vangamarthi,who had completed his intermediate came to casuality with the chief complaints of fever,body pains and weakness since 4days.
HOPI:
Patient was apparently asymptomatic 4days back and then he developed fever,body pains and weakness.Fever was intermittent,high grade fever during morning and gradually decreased by evening after taking medications,not associated with chills.H/o headache in association with fever and subsided gradually as the fever decreased.Body pains developed along with fever mostly lower limbs are painfull which was dragging type of pain and there is weakness.There is h/o abdominal pain since yesterday morning which was dragging type and localised to epigastric region.There was cracking of upper lip.
Patient had h/o fever,bloody diarrhea 1month back.Then the fever was on and off,high graded and he passed loose stools 4-5 times/day for 2days.Then he gave blood sample suspecting typhoid which was positive and then he went to nalgonda and got treated.
Past history:
No similar complaints in the past.
Personal history:
Diet:Mixed
Appetite:Decreased
Sleep: Adequate
Bowel movements decreased since 3days and regular bladder movements.Today he passed stools.
No addictions.
General physical examination:
Patient is conscious, coherent, co-operative and we'll oriented to time,place,person.He is moderately built and nourished.
No signs of pallor,icterus,cyanosis,clubbing,generalised lymphedenopathy and edema.
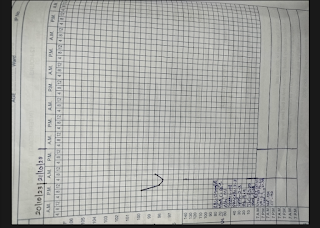
Vitals:









Comments
Post a Comment