63yr old male complaints of fever,cough since 1 month difficulty in breathing since 2 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
A 63yr old male patient came with the complaints of fever,cough since 1 months and difficulty in breathing since 2 days
HOPI
Patient was apparently asymptomatic 1 month back and then developed fever intermittent low grade relieved on taking medication associated with chills and rigor
C/o cough since one month associated with sputum sometimes
C/o difficulty in breathing since 2 days
Past history
K/C/O CAD Post PTCA status 8 yrs back
K/C/O HTN since 3 months but not on any medication
H/o blood transfusion 8 days back - 1 PRBC ,
N/K/C/O DM , CVA , Asthma , TB, Epilepsy
Personal history
Diet : mixed
Appetite: normal
Sleep : adequate
Bowel and bladder : regular
Addictions:
Alcohol - used to consume alcohol stopped 15 yrs back
H/o smoking + but stopped 15 yrs back
General examination:
Patient is c/c/c well oriented to time place person
He is ill built and nourished
Vitals :
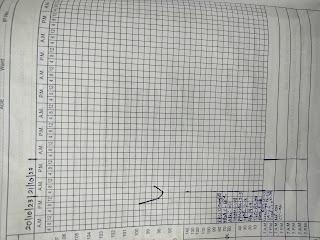
Temperature - 101 F @4pm
100 F @5pm
98.7 @6pm
BP- at 4:15pm 110/60mmHg
5:45pm 70/30mm hg
6pm 80/40mmhg(noradrenaline 4ml/hr )
6:45pm 70/40mmhg (ND - 6ml/hr)
7:30pm 70/50mmhg (ND - 8ml/hr)
8pm 120/80mmhg (ND - 8ml/hr)
9pm 120/80mmhg(ND- 7ml/hr)
PR - 96bpm
RR - 16cpm
CVS - S1 S2 heard no murmurs
RS - BAE PRESENT NVBS HEARD
P/A -Soft , non tender
CNS -NFND
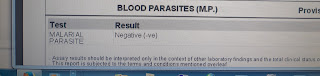
Investigations:
Provisional diagnosis:
PYREXIA UNDER EVALUATION , HEART FAILURE (EF - 54%) SECONDARY TO CAD - S/P PTCA 8yrs back
Treatment:
IV fluids : UO + 30ml/hr
Inj.NORADRENALINE (6ml/hr IV infusion ) increase /decrease according to BP - 0.16mg = 1 ml
Tab. ROVASTATIN + CLOPIDOGREL PO/HS (75MG + 10 MG )
















Comments
Post a Comment