A 65year female,came to casuality with chief complaints of decreased urine output
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitt.
A 65year old female,resident of Tondavayi,came to casuality with chief complaints of decreased urine output since 4days.
HOPI:
Patient was apparently asymptomatic 1year back and then she fell down and had injury,underwent surgery and has rod in left thigh and takes analgesics when ever she has pain.
7 days back,she had itching on back of right ankle,on further scratching blisters developed,she applied mehendi leaves on blisters which developed into a wound l,which was associated with Pain and redness and wound size increased.No history of discharge.Then they visited RMP and was given analgesics and injections and daily dressing was done.
And then urine output decreased on 8-10-22 night and on 9-10-22,morning urine output also decreased and she told her daughter in the afternoon and they went to RMP,he gave medication to increase urine output,they waited till evening and still there is no improvement and RMP suggested them to go to Nalgonda govt.hospital.
They went to Nalgonda private hospital on 10-10-22,tests were done and they identified as there is kidney problem and she need dialysis to be done,as it is not available in their hospital they referred to KIMS,Narketpalli.
On 11-10-2022,7pm they came to our hospital and tests were done and diagnosed with renal problem and planned for dialysis yesterday.
PAST HISTORY:
No similar complaints in the past.
She is not a known case of DM,HTN,Thyroid,epilepsy,TB.
SURGICAL HISTORY:
She went surgery for fall 1year back and rod was placed in her left thigh.
TREATMENT HISTORY:
H/o NSAID intake for pain after surgery.
PERSONAL HISTORY:
Diet:mixed
Appetite: Decreased since she developed wound.she is having only rice in the night.
Bowel movements are regular and decreased urine output since 4days.
No addictions.
General physical examination:
Patient is conscious,coherent,coperative and we'll oriented to time,place,person.She is ill built and malnourished.
Right sided parotid enlargement is present.
No signs of icterus,cyanosis,clubbing,lymphedenopathy and edema.
Vitals:
Temperature:Afebrile since admission but fever spike seen on 13-10-2022.
PR:82bpm
RR:13cpm
BP:160/110mmhg
Spo2:98% at room air
GRBS:90mg/dl.
LOCAL EXAMINATION OF ULCER:
On inspection:
A ulcer of about 5×4cms,over posterior aspect of ankle,spherical in shape,sloping edges and base is pale.No bleeding and discharge.
No other ulcers present.
On Palpation:
No local rise of temperature,no tenderness.
All inspectory findings are confirmed on palpation.
Floor consists of soft tissue.
Pulses present.
No lymphnode palpable.
Provisional diagnosis:Traumatic ulcer over ankle.
Treatment:
Regular dressing with left limb elevated.
Tab.CHYMORAL FORTE-TID
Tab.TAXIM 200mg per oral,BD.
Tab.METROGYL 500mg per oral,TID.
SYSTEMIC EXAMINATION:
CVS:S1,S2 Heard,no murmurs
RS:Bilateral air entry present.NVBS heard.
On inspection:
Chest wall-symmetric
Trachea-midline
No drooping of shoulders and no supraclavicular and infraclavicular hollowing.
No winging of scapula.
No sinuses,scars and dilated viens.
On percussion:
Resonant note heard and liver dullness heard on right 4th ICS.
On auscultation:
NVBS heard.bilateral air entry present.
Per abdomen:
On INSPECTION:
Franks:Free
Umbilicus:shape-slit
Skin over abdomen normal,no sinus,no scars.
No visible peristalsis.
No hernial orifices.
On PALPATION:
Local rise of temperature,no tenderness.
All inspectory findings are confirmed by palpation.
Liver is palpable,non tender
Spleen is non palpable and non tender.
On PERCUSSION:
Fluid thrill and shifting dullness is not present.
On AUSCULTATION:
Bowel sounds are heard.
CNS:No focal neurological deficits.
Investigations:
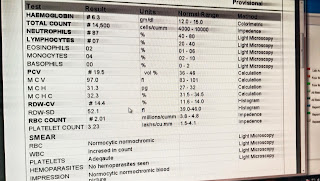
On 11-10-2022,
On 13-10-2022,
Provisional diagnosis:
On 12-10-2022,
CHRONIC KIDNEY DISEASE (CKD).
TREATMENT:
Tab.TAXIM -200mg,per oral,BD.
Tab.METROGYL-500mg,per oral,TID.
Tab.CHYMEROL FORTE,per oral,TID.
On 14-10-2022,
PROVISIONAL DIAGNOSIS:CHRONIC KIDNEY DISEASE,secondary to NSAIDS.
Inj.LASIX 40mg,iv BD
Tab.RANTAC 150mg,er oral,OD
INJ.CEFTRIAXONE 1g,iv,BD
Tab.CHYMEROL FORTE,per oral,TID
Tab.NODOSIS 500mg,per oral,BD
Tab.SHELCAL,per oral,OD
Tab.OROFER XT,per oral,OD.






























Comments
Post a Comment