A 32 yr male came with the complaints of Fever since 7 days
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
A 32 yr old male came with the complaints of fever since 1 week
HOPI
Patient was apparently asymptomatic 1 week back and then developed fever which was sudden in onset gradually progressive high grade associated with chills and generalised weakness for which he went to local RMP and took medication for 2 days still the symptoms didnot subside and further investigation like blood test done and his blood sugars were 300mg/dl
As the symptoms didnot subside they went to Miryalagudam hospital there USG was done and impression showed HEPATIC ABSCESS
and refered to our hospital
Patient came to hospital yesterday and USG was done impression showing:
NO H/o vomitings
No h/o cough cold diarrhoea
Past history:
K/c/o DM type 2 since 2 months and was on metformin hydrochloride
N/kc/o HTN TB Epilepsy BA
Personal history:
Diet mixed
Appetite normal
Sleep Adequate
Bowel decreased since 3 days and passed stools yesterday
Bladder movements are regular
Addictions: occasional alcohol consumption since 5 years but stopped consumption from 2 months
Occasionally smoker since 5 years
General examination
Pat is c/c/c well oriented to time place person
He is moderately built and nourished
No signs of pallor icterus cyanosis clubbing lymphadenopathy generalized edema
Vitals
Temperature - 102 F
BP - 110/70 mm hg
PR - 86 BPM
RR - 16 cpm
Systemic examination
CVS - S1 S2 Heard no murmurs
RS - BAE + NVBS
CNS : NFND
PER ABDOMEN EXAMINATION:
Inspection:
Shape of the abdomen:Distended
Flanks:Free
Umbilicus:center,oval shape
Skin-normal,no sinuses,scars,striae
No dilated viens
Abdominal wall moves with respiration
No hernial orifices
Palpation:
No local rise of temperature,no tenderness.All inspectory findings are confirmed by palpation.
Liver:Not palpable,Non tender,no hepatomegaly
Spleen:Not palpable,non tender,no splenomegaly
Kidney:Non tender and not palpable
No other palpable swellings
Percussion:
On abdomen percussion tympanic note is heard
Liver span:12cms in mid clavicular line
Spleen:No dullness is heard
PROVISIONAL DIAGNOSIS:
HEPATIC ABSCESS
K/C/O DM TYPE 2
INVESTIGATIONS:
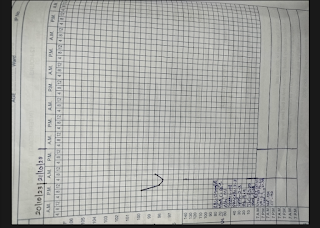
USG DONE on 7/10/23
Impression: Hepatic abscess of size 9x7 noted in 5 and 6 segments of liver with 20% liquefaction
TREATMENT:
Inj.NEOMOL 1G IV STAT
Inj.MAGNEX FORTE 1.5GMS IV STAT
Inj.METROGYL 500MG IV TID
Inj.PAN 40MG IV/OD
IV FLUIDS - NS RL
Tab.DOLO 650MG PO/SOS
TEPID SPONGING










Comments
Post a Comment